Viruses, BiTEs, and T-cells: A Triple Threat to Tackle Cancer:
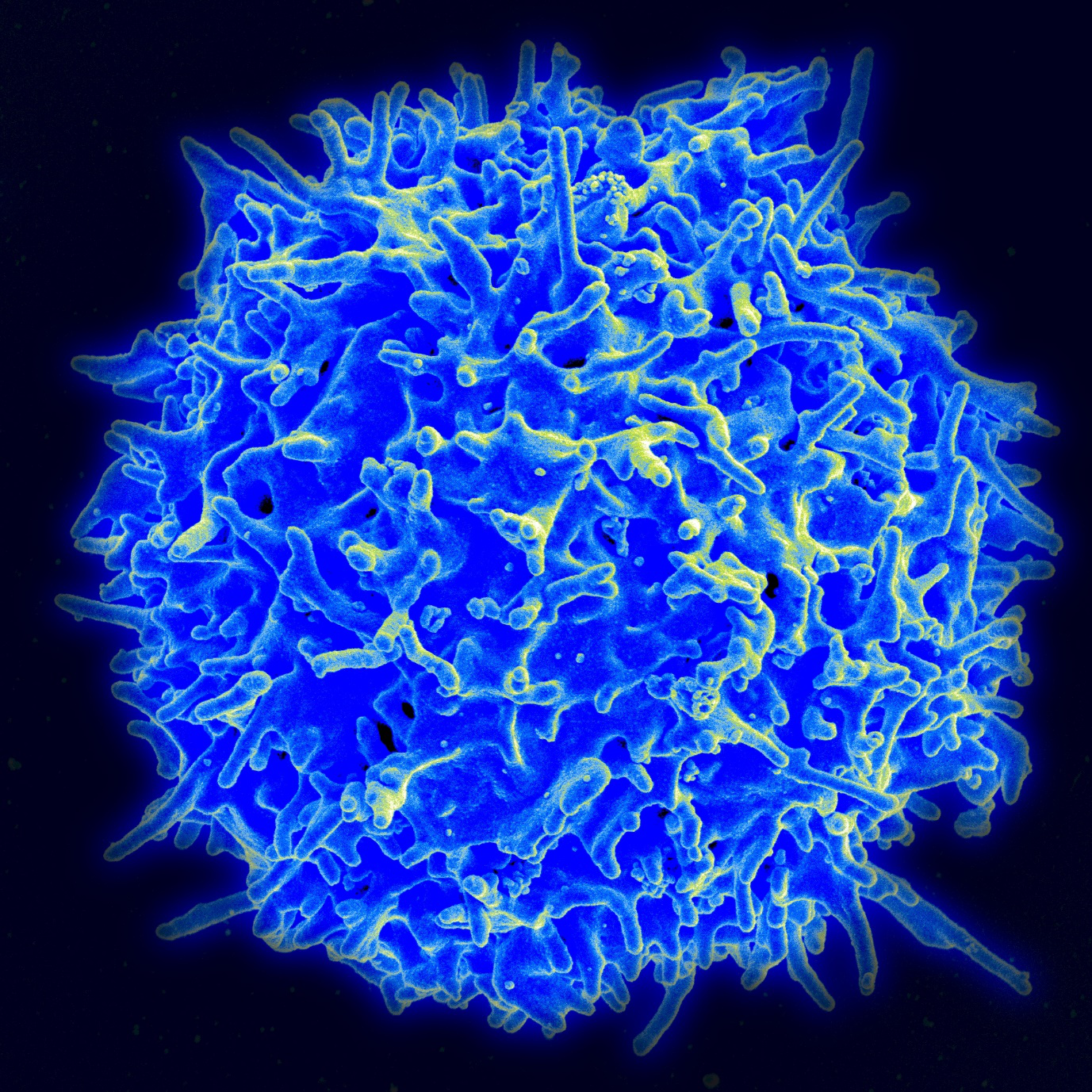
CAR-T takes T-cells, cells which seek out and/or destroy disease in the body and uses synthetic DNA to alter them so they can recognize cancer cells via a specific protein (of the scientists choice) on the cancer cell surface. When put back into the patient the CAR-T cells can now seek out cancer cells and destroy them by signaling the bodies own immune system to attack cancer, much like it would an infection. This one of the most promising new cancer therapies available, with the first drug of its kind (Kymriah), approved last year.
However, CAR-T is not without fault. The study highlights two major issues with CAR-T, using T-cells which seek out Folate receptor α (FRα), a protein on the surface of several cancers including ovarian3. First, they show that the CAR-T cells select for tumour cells which don’t have FRα, killing the ones with it and leaving a population without FRα behind; this essentially “evolves” a tumour to escape the treatment. Second, the tumour is often an immunosupprthe essive environment, in other words: the immune system doesn’t work properly inside a tumour. This can cause the CAR-T cells to get “switched off”, preventing them from signaling the immune system to destroy the tumour even though they have successfully found cancer cells.
To solve problem one the authors wanted to give the CAR-T therapy a second way of targeting cancer, the hope is that the tumour would not be able to escape by selecting for a population without both types of cancer marker. They chose EGFR (Epidermal Growth Factor Receptor) as their second cancer-specific target. Like FRα, EGFR is found on the surface of many cancers. They also wanted to be able to stimulate normal T-cells to attack the tumour as well. The solution they chose is a therapy called a called a Bi-specific T-cell Engager, or “BiTE”.
BiTE’s (Figure 1) are derived from antibodies, the body’s natural way of labeling harmful cells, like bacteria or virus-infected cells, for destruction by the immune system. The BiTE in the study is designed to stick only to two types of molecule: EGFR (On Cancer) and CD3 (on T-cells). The BiTE’s physically stick the T-cell to the cancer cell “showing” it where to direct the immune system.
We are left with the second problem: How to stop the tumour switching off the immune system. The solution is from the nascent field of Oncolytic virology; a promising, fast-growing field which uses genetically engineered viruses to fight cancer. The viruses are engineered so they can’t damage healthy cells but are deadly to cancer. They have the bonus of causing inflammation (damage signaling) in the cells they infect, which activates the immune system. Normally this would be a bad thing, but since the only cells the virus is infecting are within the tumour it works in the therapy’s favor.
An Oncolytic Adenovirus (OAd) was altered to carry the DNA of the EGFR-CD3 binding BiTE. When the virus seeks out the cancer cells it infects and forces them to make BiTEs. The BiTEs then stick to both T cells and cancer, bringing them together. Since the tumour is now also displaying damage signaling because of the virus, T-cells become activated and attack cancer.
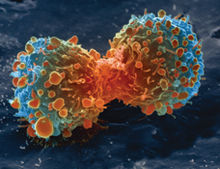
The authors showed in a mouse model of colorectal cancer that the BiTE expressing virus alone was ineffective. On its own, the CAR-T enabled 40% of mice to survive (compared to none in the untreated mice), but the combination of CAR-T + OAd-BiTE saved 100% of the mice. Excitingly the authors showed similar results in a mouse model of pancreatic cancer, which has a notoriously poor prognosis.
All the therapies used in this study are very new and hold individual promise for combatting cancer. While the approach in this study is still far from human trials it holds great potential. By combining our knowledge of therapies from different scientific disciplines, whether it be virology, cell therapy, or immunology, we can find synergistic effects like this one. As our understanding of cancer grows we can refine these exciting new technologies even further and seek out new combinatorial effects to achieve even better outcomes for patients.
To have a complete look at the article join us on “International Conference on Cell and Gene Therapy” on October 15-17,2018 at Vienna, Austria.
Go to the link: Gene Therapy conference
Comments
Post a Comment